
SADIMoD
Background
Drug-induced movement disorders
The long-term treatment for psychiatric diseases is frequently complicated by the occurrence of movement disorders. These movement disorders may be drug-induced, related to psychiatric disorders, or to a concomitant neurological disorder. It is necessary to accurately measure the severity of these movement disorders, while studying the efficacy and safety of psychotropic drugs.
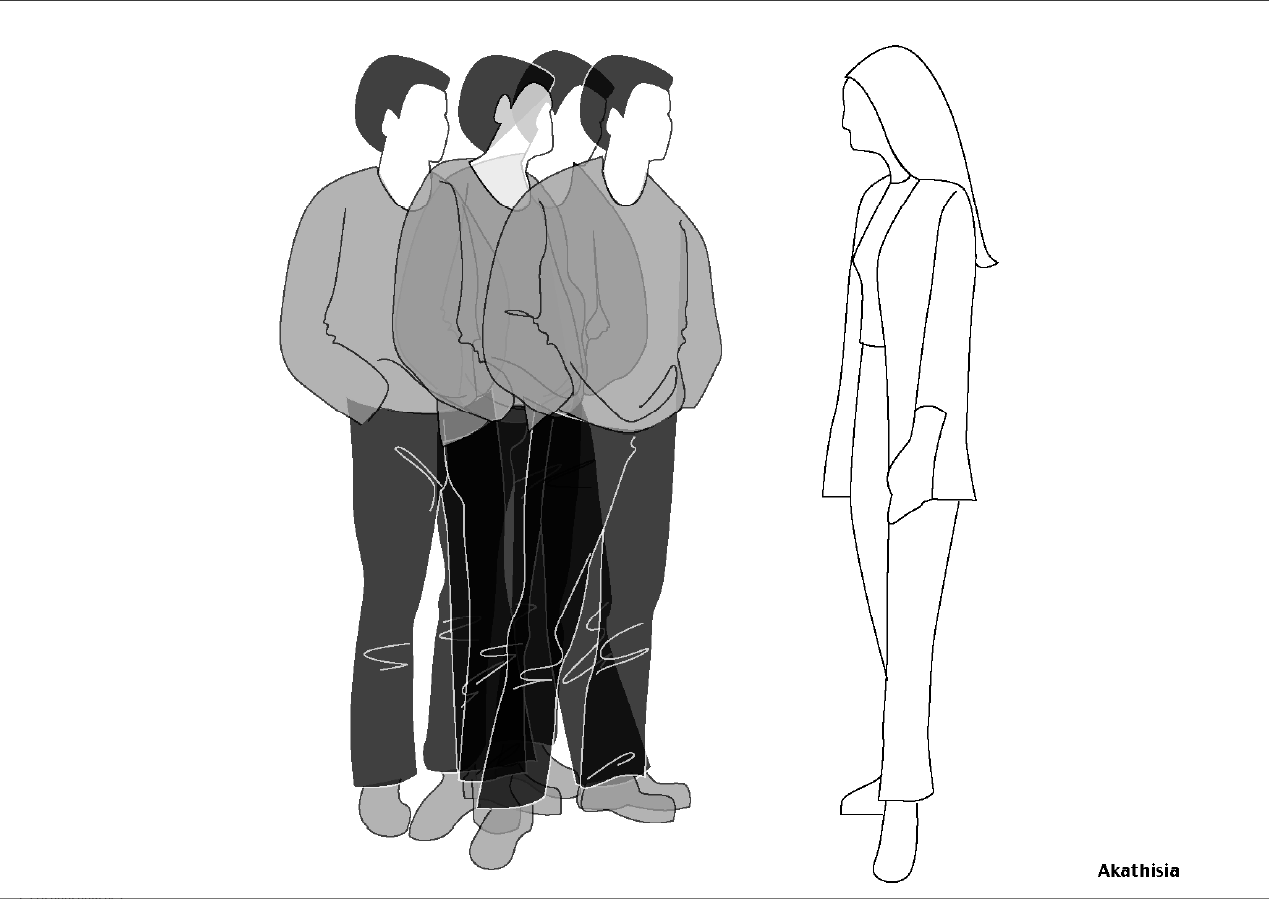
Akathisia
Akathisia consists of subjective as well as on objective symptoms. It is primarily, but not exclusively affecting the legs;
Characteristics of this subjective experience are: the perception of a foreign but nevertheless inner compulsion to move resulting in a sensation of restlessness, nervousness, “feeling itchy”
Objective motor symptoms are an increased, abnormal frequency of movements that often are complex and stereotype. The patient may consciously suppress these movements.

Ataxia
Ataxia is the absence of orderly and accurate moving, without a substantial decrease of the control of movements due to muscular weakness.
With ataxia the symptom is a disorder of the tonic voluntary and reflexive muscular contractions, that are essential for maintaining posture and balance (static or posture ataxia) and a change in direction and extend of voluntary movements (dynamic or movement ataxia).
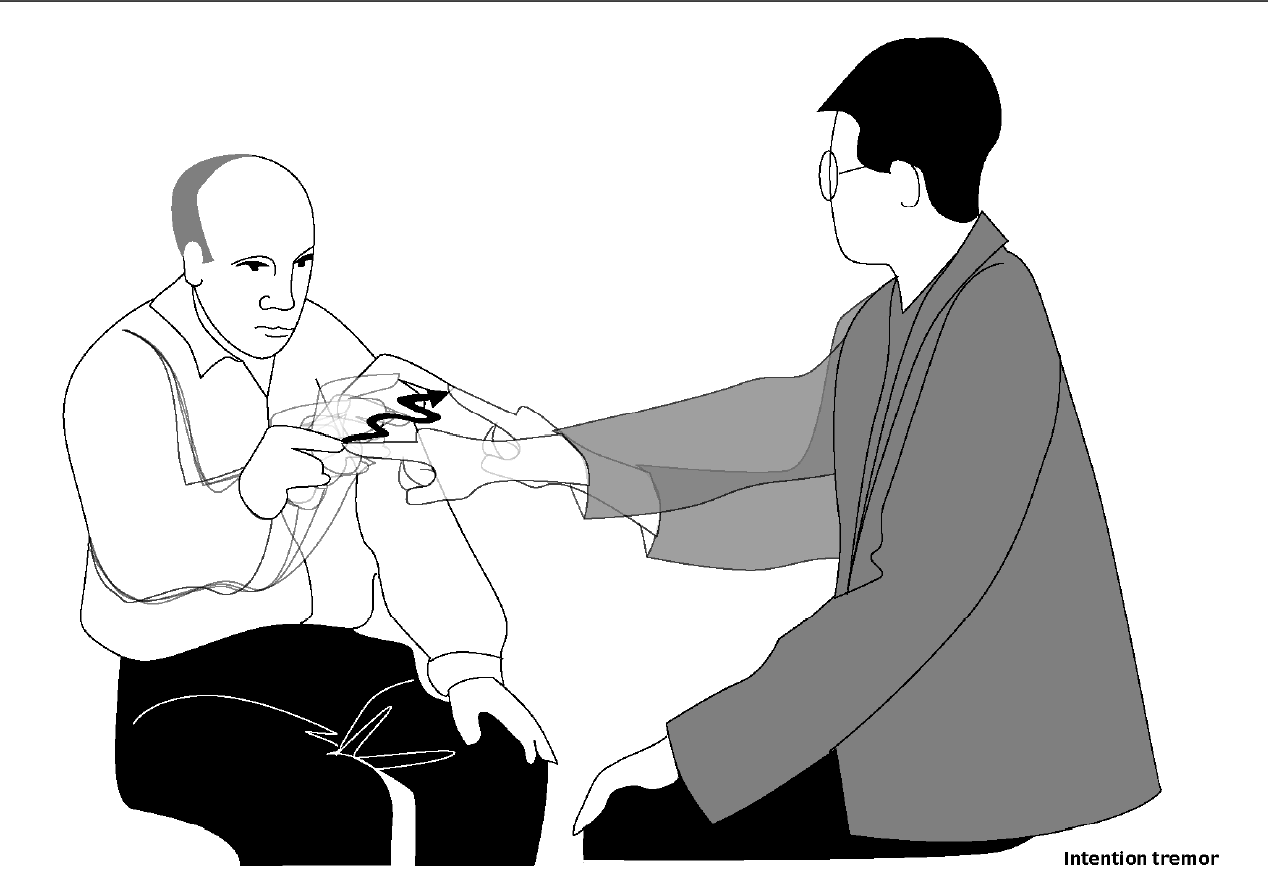
Tremor
Tremors are frequent, rhythmical and continuous pendular movements in one or more vibratory planes, without vibration free intervals. They wax and wane in amplitude, but the frequency does not change in any one patient. They are often asymmetric and can affect all parts of the body.
They are subdived into: rest tremor, intention tremor and postural tremor

Dystonia
Dystonia is a syndrome of continuous contractions of often antagonistic muscle groups (spasms) causing slow twitching, repetitive movements (lasting > 2 sec) or an abnormal posture.
Many dystonic movements are action-specific. This means that they are connected to a certain provoking factor, the execution of a specific motor task.
Touching a specific dermal area or supporting an affected part of the body may, subjectively or objectively, causes relief of the complaint (sensory tricks).
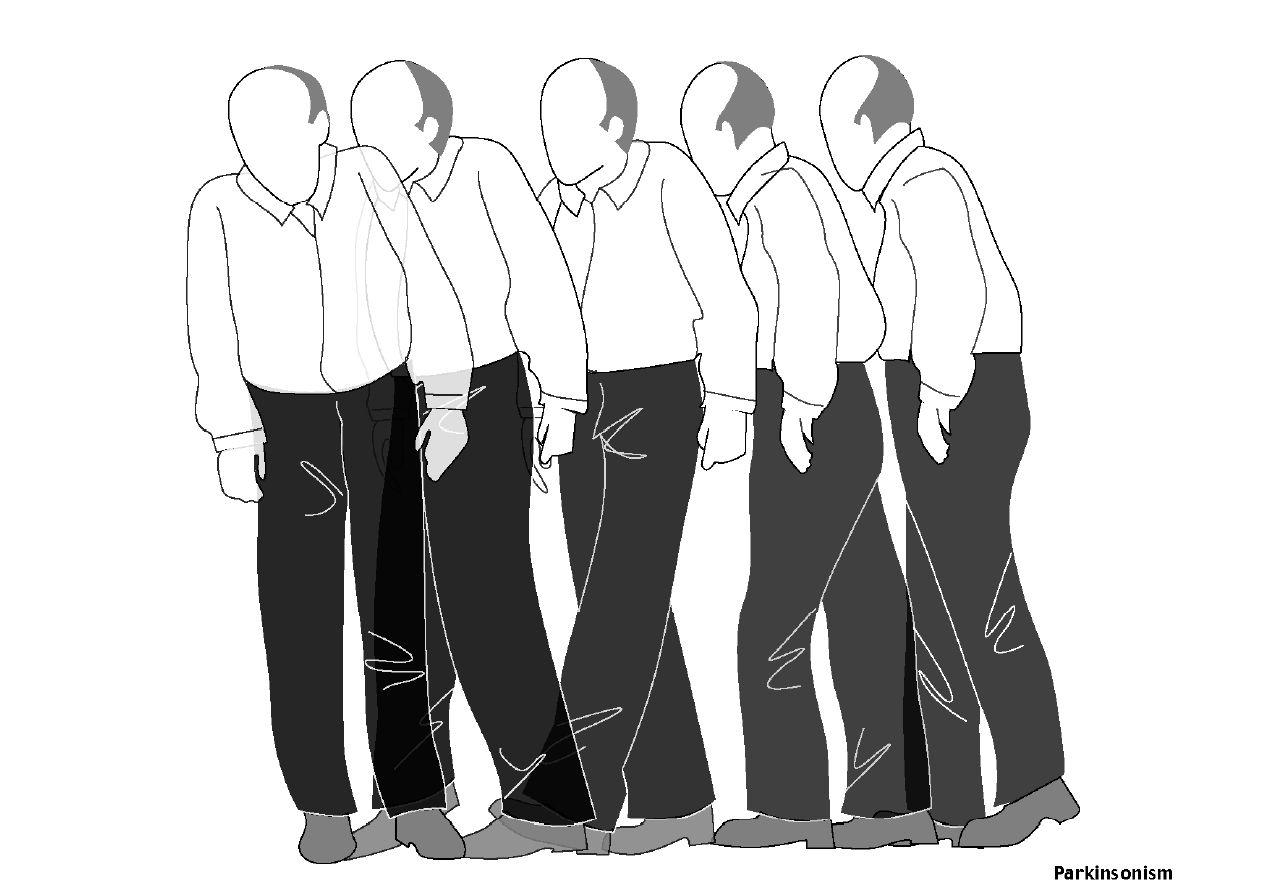
Parkinsonism
Parkinsonism is a syndrome that, regarding its symptoms, shows a resemblance with Parkinson’s disease. Akinesia is a prime aspect. Hypertonicity and autonomous phenomena are observed less frequent, usually later and/or in more serious cases. The typical Parkinson-tremor often develops in a later stage and is relatively uncommon in drug-induced Parkinsonism.
The bradykinesia, hypokinesia and akinesia manifest themselves in a reduction and/or slowing down of spontaneous movements (shutting/raising of the eyelids), associated movements (swaying arms during walking) and wanted movements.
Rigidity is often preceded by symptoms such as weakness and pain. In passive bending and stretching of the arm a plastic resistance (rigidity) is felt over the entire trajectory. Also rhythmic fluctuations of the resistance are felt (cogwheel phenomenon).
Autonomous symptoms include hyper-salivation (drooling) and seborrhoea (oily skin).
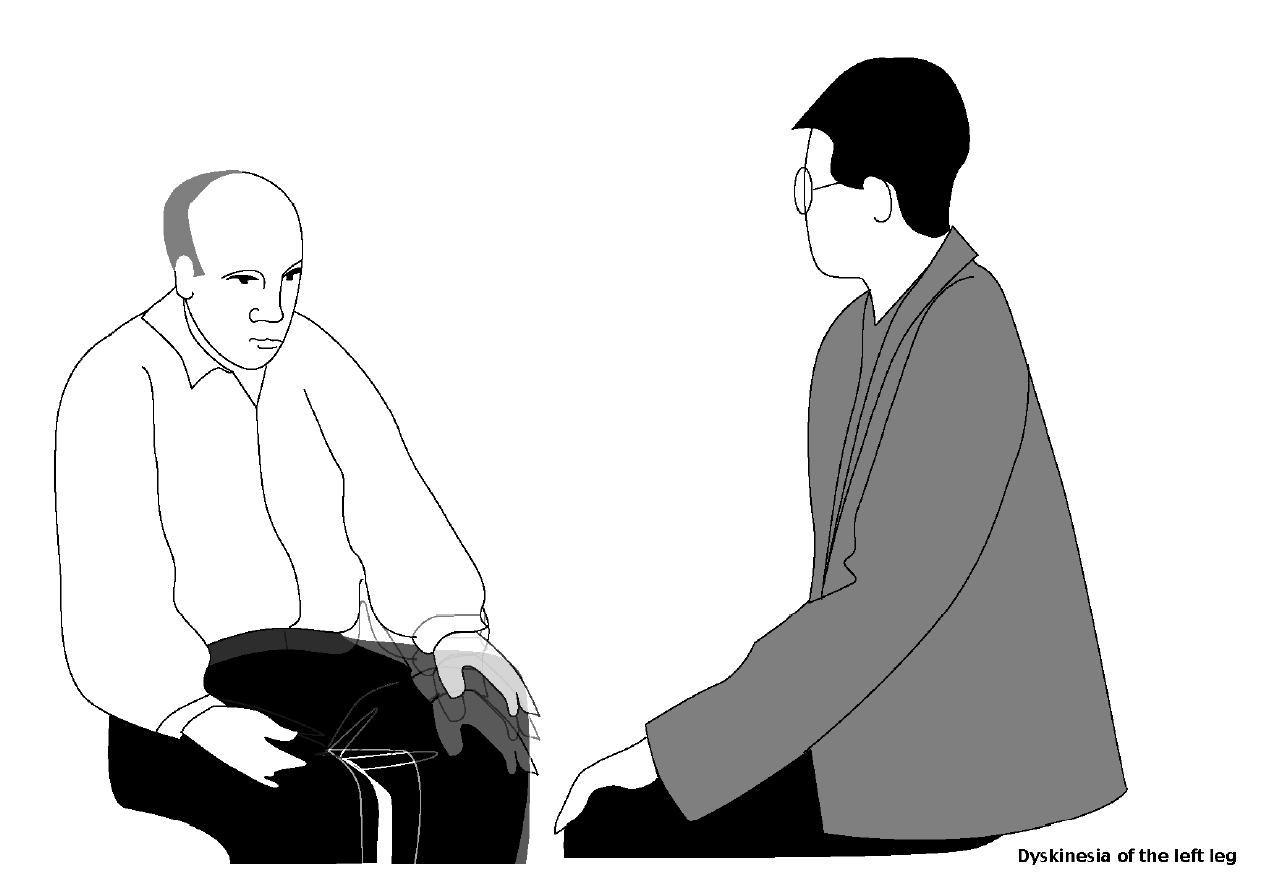
Dyskinesia
Dyskinesia is a collective name for a complex of involuntary hyperkinetic movements. The movements are irregular, repetitive, and usually with motionless intervals. The dyskinesia is reduced when the muscles are used voluntary and when the attention is focussed on it. They increase during activity and in anxiety.
The most widely described phenomenon comprises the facio-bucco-linguo-masticatory (BLM) syndrome, which consists movements of the lips, jaw, tongue and eyelids.
In addition, dyskinesias present themselves as choreiform movements of the extremities and distal athetosis. These movements consist of irregular or twisting movements of the fingers, the feet, and the toes.
Rating scales for movement disorders
For research purposes, it is nowadays common practice to use a combination of the Simpson and Angus’s Rating Scale for Extra pyramidal Side Effects (SEE), the Akathisia Rating Scale of T. Barnes (BAS) and the abnormal involuntary movement scale (AIMS) of the National Institute of Mental Health (NIMH). Other researchers use a composite scale such as the Extra pyramidal Symptom Rating Scale (ESRS) of G. Chouinard and A. Ross-Chouinard or the Sct. Hans Rating Scale (SHRS) of J. Gerlach.
Limitations of existing scales
However, the SEE and the AIMS show important limitations that limit their validity and reliability (especially in long-term trials). Moreover, the objective of the available instruments is to measure the involuntary movement syndromes independently. In most cases no explicit criteria are given to distinguish different disorders and the rules to examine the patient are sometimes conflicting. On top of that, definitions for severity scores are often absent. We therefore, decided to create a new test. In addition we developed a strictly standardized examination schedule that is suitable to reveal the presence of involuntary movements in a reproducible manner.
SADIMoD
The first Dutch version of the SADIMoD appeared in 1994, and the last English version in 2000. It can be considered to be an expansion of the Sct. Hans Rating Scale for Extra pyramidal Syndromes. We implemented slightly modified versions of the AIMS (items 1-7), the BAS and the Fahn-Marsden Dystonia Scale. We added three new subscales: one for the assessment of various tremors, one for the assessment of ataxia, and one for the global assessment of relevant psychic symptoms. When absent in the original scales, the item definitions were taken from the UKU Side Effect Assessment Scale. In the case of the Parkinsonism subscale this was Webster’s Parkinson Disease Rating Scale for Symptoms and Signs. The writing test was obtained from H.J. Haase. The questionnaire brings the necessary information to complete the various subscales. By applying its answers the original complete AIMS can be reconstructed.
Structure of the SADIMoD
Overview
The SADIMoD exists of a standardised examination schedule, a questionnaire, a writing test, a rating form, and a glossary with the criteria for the classification of different movement disorders and the definitions of severity scores.
Examination schedule
The examination should be conducted in such a manner, in a fixed sequence and within a fixed setting, that it can be reproduced. To be able to compare the severity of the disorders in long-term trials the making of a recording on videotape is a simple solution. This videotaping makes a retrospective, and even blind, assessment by several observers possible. However, in relatively short-term trials of a few months duration, the life scoring of patients by single raters is certainly sufficient.
Questionnaire
The questionnaire is intended to collect information about subjective complaints and paroxysmal phenomena. The answers should be used to score the relevant disorders. Moreover, they can serve to reconstruct the original AIMS. The examiner should adequately explain the phenomena and verify the answers. The questionnaire should overrule all remarks made during the examination.
Writing test
The writing test is included in order to obtain a sample of the hand writing. This sample should be used while scoring hypokinesia, tremors or ataxia. The analysis according to H.J. Haase is optional.
Disorders may not be absolutely clear from the video-registration made during the test. The examinor is encouraged to write specific observations on the ‘Remark’ form.
Rating form
The rating form contains subscales for akathisia, ataxia, dyskinesia (during activity and in rest, separately), dystonia, parkinsonism, psychic symptoms and tremors. These disorders are defined in the manual. Each subscale also contains a ‘Global impression’ item which is also intended to offer the opportunity to express doubts concerning the nature of the observed disorder. All subscales are dealt with independently during analysis.
The items are scored on a scale of zero (absent) to four (severe). A score of ‘one’ is used in the case of uncertainty. The original structure of the Fahn-Marsden Dystonia Scale is preserved in the Dystonia subscale.
Instruction Video
The authors made an instruction video, that is also available on YouTube. It is intended to be used by clinicians to get trained in applying the SADIMoD in order to examine and rate their patients. A general instruction is given with some background information and several details on how to deal with specific problems. Moreover, the SADIMoD examinations of three patients are present. These can serve to learn how the patients should be examined and how the video-registration should be made. Details on these examinations and the corresponding scorings are given in the manual. The latter can be used to compare their results to.
SADIMoD Forms
You can download the SADIMoD forms by clicking on the links
Questionnaire and writing test
We would greatly appreciate when you would contact us when you notice any mistakes or typing errors in the forms.
Documentation
The characteristics of the SADIMoD are described in two publications. In order to download a pdf of these articles, please click on the titles: